Amid a wave of new COVID-19 cases driven by highly infectious subvariants, hospitalizations in Los Angeles County hospitals have surged to nearly 1,000 – a rise of more than 200 patients in the last four days alone. Given current trends, the Los Angeles Department of Public Health (Public Health) announced Thursday that the county may have to reimpose mandatory indoor masking by the end of the month.
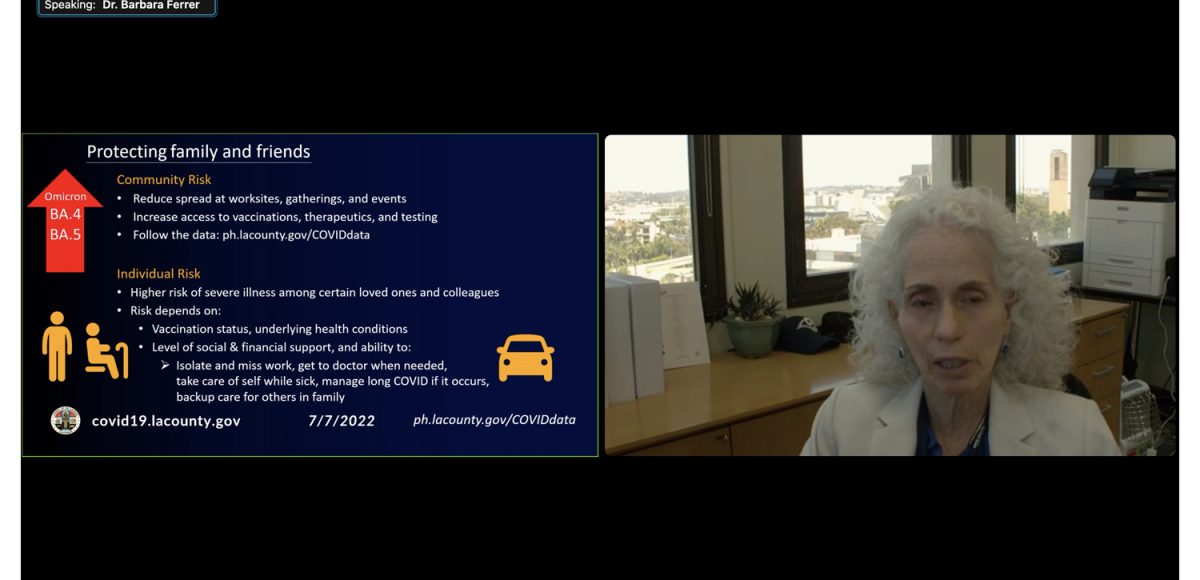
“As we face a fresh wave of new rising subvariants, we do remain focused on preparedness for what may come next,” Public Health Director Dr. Barbara Ferrer said at a press conference on July 7. “LA County, as you all know, is always working on building and maintaining preparedness in the five key areas: surveillance, access to vaccines, access to testing, access to therapeutics, and outbreak management.”
Public Health has reported a total of 3,143,536 positive cases of COVID as of July 5. A total of 9,737 Beverly Hills residents have contracted the disease, 45 of whom have died.
Hospitalization rates reached a nadir of 209 in April but have been ticking up in the subsequent months to the current number of 989.
Ferrer said Public Health expects hospitalization rates to exceed 10 admissions per 100,000 people by the middle of the month, which would push the county into the CDC’s high community level designation.
“Should we remain in the high community level designation for two consecutive weeks, universal indoor masking and alignment with CDC would be implemented across LA County,” Ferrer said.
The soonest the county could reimpose indoor mask requirements would be July 28, assuming the trends continue. Ferrer stressed, though, that she could not predict when or if the county would move to the high level of transmission but could only project “based on the rate of increase in admissions over the last two weeks.”
Other counties, including Ventura, have declined to reinstate mask requirements. Ferrer stood by masks as a “simple and effective tool” that, while “not perfect,” will “help slow transmission.”
She added that plenty of places still require indoor masking, including public transit, congregate care facilities, prisons and jails, and even Public Health.
Ferrer also noted that the county is seeing a slight uptick in COVID-positive deaths for the first time “since the winter surge.”
“Five out of the past seven days we have reports of 10 or more deaths,” she said.
The Los Angeles County of Public Health began warning of the growing spread of two subvariants of the Omicron strain of the virus before the July 4 holiday.
“Given the rising number of COVID cases and hospitalizations, and the increased circulation of the more infectious BA.4 and BA.5 subvariants, it is extra important to take steps that reduce the risk of transmission especially over the long holiday weekend; this helps us protect ourselves, our families, and our community,” Public Health Director Dr. Barbara Ferrer said at the time.
At the press conference, Ferrer said that Omicron accounted for 100% of sequenced cases, with BA.4 and BA.5 growing in prevalence.
With the holiday weekend in the rearview mirror, officials anticipate more cases in the coming days. Ferrer stressed the steps that people can take to reduce risk, which she described as a “collective responsibility.”
“To slow down spread, we can wear masks when indoors, test when gathering and stay home and away from others if we’re sick or we’ve tested positive, to reduce stress on the health care system and the worst outcomes associated with COVID. We can get vaccinated and boosted and help those around us get their vaccinations and boosters.”
As the pandemic drags on into its third year, researchers are starting to uncover the profound impact the virus has had on general health and welfare. According to a National Cancer Institute study published Tuesday, COVID has become the leading cause of death among Americans between the ages of 45 to 54. The study found that COVID was the third leading cause of death in the United States between March 2020 and October 2021.
Another study in the Journal of the American Medical Association calculated that overall life expectancy for Californians fell about three years as a result of the pandemic. The study added to a growing body of research finding that the virus impacted marginalized communities harder than socioeconomically well-off communities.
“Our findings are another troubling sign of how the pandemic’s impact was not felt evenly across all communities,” Till von Wachter, a UCLA professor of economics and study co-author, said in a statement.